This Policy Brief from APF Canada's Distinguished Fellow, Dan Ciuriak, focuses on the question of the international transmission of information concerning the outbreak of the COVID-19 pandemic in Wuhan – who knew what when. In contrast to the dominant narrative, this review establishes, based on published information outside of mainland China, that the policy-relevant information as of 31 December 2019 concerning that outbreak had spread worldwide and was sufficient to frame the necessary preventative responses, which to this date remain essentially the same (namely the routine precautions advised for any airborne respiratory diseases).
Further, notwithstanding the mix of good and poor responses to the pandemic in different jurisdictions, and regardless of the response in Wuhan, global transmission was a sealed deal because of the stealth nature of COVID-19. Moreover, the scale of the pandemic in individual countries is largely a function of choices made independently by governments and populations around the world based on the same and sufficient information.
INTRODUCTION
Was the pandemic preventable? This is a question that continues to be much debated, in the public discussion on social media, through think tank reports and in commentaries; as part of the political blame game, [1] including implicitly through the call for an inquiry into the origins of the pandemic (Lester, 2020); and even in legal deliberations pursuant to lawsuits brought against China for various alleged failures, including delays in responding to a known epidemiological threat, allowing (or even convening) mass gatherings with the fore-knowledge of mass contagion risk, lack of transparency in recording and reporting infection rates among the population, failing to share important public health information with other countries, and hoarding personal protective equipment (PPE) (Keitner, 2020).
One would think, therefore, that the basic facts of the international transmission of the information on the coronavirus, COVID-19, would be consistently reported and there would be little controversy on this point – even if the understanding concerning the international transmission of the virus itself remains a work in progress. This, however, is not the case.
Most charitably, this may reflect a massive proliferation of commentary that led to a “loss of signal” as one commentary cited earlier commentaries, resulting in derivative statements that deviated substantively from the original documents. This does happen. Less charitably, this may reflect deliberate disinformation where information from different time periods is juxtaposed to invite the reader to draw incorrect inferences concerning what was known, when it was known, and by whom it was known. This too does happen.
This note reviews breaking news reports, original notices issues by official agencies, and the statements of various organizations around the world at the time the outbreak was first reported. These first reports and initial reactions are not at all influenced by the subsequent commentary that evolved in the context of geopolitical frictions, and which served to create new and alternative facts. The note also notes the subsequent findings concerning the coronavirus, including its early spread through ex post forensic exercises, and draws conclusions from those findings.
To preview the main conclusions, there are three: (a) there was no “information asymmetry” internationally concerning the outbreak in Wuhan at the time that policy decisions had to be taken; (b) the policy-relevant information on hand as of 31 December 2019 concerning that outbreak was – surprisingly – sufficient to frame the necessary preventative responses, which to this date remain essentially the same; and (c) notwithstanding the mix of good and poor responses to the outbreak in different jurisdictions, global transmission was a sealed deal because of the stealth nature of COVID-19. On the latter point, the pandemic was not likely preventable. Moreover, the scale of the pandemic in individual countries is a function of choices made independently by governments and populations around the world based on the same, sufficient, and early information.
BREAKING NEWS

30 December 2019: The First Posted Notice from Wuhan Medical Authorities
On 30 December 2019, the Wuhan Municipal Health Commission issued an urgent notification to medical institutions under its jurisdiction, ordering efforts to appropriately treat patients with pneumonia of unknown cause. This information was in the public domain. This can be easily confirmed since, on the morning of 31 December 2019 in China, a China Business News reporter called the official hotline of Wuhan Municipal Health and Health Committee to verify the information. Finance Sina Mobile published the story, which was in turn picked up the Program for Monitoring Emerging Diseases (ProMED) run by the International Society for Infectious Diseases (ISID) in Brookline, Massachusetts. ISID reposted the report just before midnight (23:59) on 30 December in North America (ISID, 2020).
This report contains some illuminating information. Four of the cases of pneumonia that could not be diagnosed presented with the following symptoms: fever (greater than or equal to 38C); imaging characteristics of pneumonia or acute respiratory distress syndrome; reduced or normal white blood cells in the early stages of onset; a reduced number of lymphocytes. After treatment with antibiotics for 3 to 5 days, the condition had not improved significantly (ISID, 2020).
Accordingly, even before the first official reports through the World Health Organization (WHO), the information of a pneumonia of unknown cause that does not respond to treatment and that warranted an urgent notice from local health authorities with a counsel to take “appropriate” measures has gone around the world and had been picked up and reposted by monitoring agencies established precisely for that purpose.
31 December 2019: The First Official Report
The following day, on 31 December 2019, at 1:38 p.m., the Wuhan Municipal Health Commission made the first official report to China’s WHO office in Beijing on “multiple pneumonia cases.” This report had several notable facts:
- Twenty-seven cases had been identified.
- Of these, seven were described as “severely ill.”
- The remaining cases were described as “stable and controllable,” with two cases described as “getting better and … scheduled to be discharged in the near future.”
- The clinical manifestations of the case were “mainly fever, a few patients had difficulty breathing, and chest radiographs showed infiltrative lesions of both lungs.”
All cases were treated in isolation, contact tracing was reported to be in progress, and hygienic investigations and “environmental hygiene treatment” was being applied in the South China Seafood City, which had been linked to the cases. The report mentions consultation of “clinical medicine, epidemiology, and virology experts in Tongji Hospital, Provincial Center for Disease Control, Wuhan Institute of Virology, Chinese Academy of Sciences, Wuhan Infectious Disease Hospital, and Wuhan Center for Disease Control, etc.”
Further, based on the epidemiological investigation, preliminary laboratory analysis and other aspects of the situation, the Wuhan official report suggests that the cases involved viral pneumonia. Based on this preliminary diagnosis, the report goes on to advise that “the disease can be prevented and controlled by preventing indoor air circulation, avoiding public places where there is no air circulation and places where people are concentrated, and wearing masks when going out.”
So before this became a global issue, the Wuhan/Hubei infectious disease community as well as the local hospitals are stated as having been consulted and advised to treat it as an infectious airborne disease; and, the specifics were more or less exactly what is currently advocated worldwide (see e.g., Campbell, 2020) (because it is not specific to COVID-19 but to the generic infectious airborne disease of which COVID-19 is but one):
- prevent indoor air circulation,
- avoid public places with no air ventilation,
- avoid crowds (social distance), and
- wear masks.
This looks like boilerplate Virology 101. To be sure, the Wuhan investigation reported that “no obvious person-to-person transmission” had been found and that “no medical personnel have been infected.” However, these statements, which have been repeated endlessly, must be seen in the context in which they were made: matter-of-fact reporting, without particular emphasis, in a context in which “the detection of pathogens and the investigation of the cause of infection are in progress,” and in which the actual guidance as to procedural protocol was to treat it as infectious.
COVID-19 Information Goes Global
When Hong Kong Knew
The Wuhan official report came out on New Year’s Eve, so it might be expected to have been overlooked. That was not the case. On 31 December, the South China Morning Post, published in Hong Kong, reports on this development under a headline “Hong Kong takes emergency measures as mystery ‘pneumonia’ infects dozens in China’s Wuhan city.” What were Hong Kong officials thinking? They were thinking SARS and Avian flu – that is, previous outbreaks of deadly viral influenza that was contagious. What did they do? They moved to “step up border screening and put hospitals on alert.” (Zuo et al., 2019).
The South China Morning Post article cites the key statistics from the Wuhan report: twenty-seven cases, seven serious, and two recovering, confirming that the Hong Kong reporters were reading the Wuhan report.
It is also relevant to note the reaction of health care authorities and experts outside of mainland China. As regards Hong Kong health authorities, they were cautious:
“The situation in Wuhan is unusual, and we are not sure about the reasons behind the outbreak yet,” said Secretary for Food and Health Sophia Chan Siu-chee after an urgent night-time meeting with officials and experts on New Year’s Eve. “Since we are now in the holiday season, and Hong Kong has close transport ties with Wuhan, we must stay alert.” (Zuo et al., 2019).
Meanwhile, microbiologist Yuen Kwok-yung from the University of Hong Kong notes the similarities with the 1997 Avian flu and the 2003 SARS episode and then goes on to offer some opinions on the seriousness of the situation:
“But there’s no need to panic. First, compared with 2003, we have better systems in notification, testing and infection control. We also have medicines that we can try … In the past, we didn’t have proper isolation facilities. If you ask me will there be any chance that the severity will be the same as in 2003, I will say the chance is low. All we have to do is to be on alert.”
When Taiwan Knew
But Hong Kong was not even the first jurisdiction outside of Mainland China to react. According to Taiwan’s Vice Premier Chen Chi-mai, Taiwan can claim that honour. During an Executive Yuan briefing at 8:00 a.m. on 31 December (i.e., before the Wuhan report to China’s WHO office), Chen reports that he informed Premier Su Tseng-chang of the developments in Wuhan (OCAC, 2020). According to Chen, an inter-ministerial meeting was held an hour later leading to immediate activation of stricter border control measures, including stepping up testing of incoming travellers who had a fever, questioning suspected cases about travel and contact history, and implementing health screening of passengers arriving on direct flights from Wuhan prior to deplaning, starting that same day, 31 December 2019.
Taiwan’s Center for Disease Control (CDC) adds further information: “The Department of Disease Control has confirmed the information of the epidemic with the Chinese Center for Disease Control and Prevention and the World Health Organization (WHO) IHR window today (31).” The CDC report repeats the key statistics from the Wuhan report: “27 cases of pneumonia have been found in the local area recently, 7 cases are in critical condition, all have been isolated and treated, and 2 cases have improved.” Further, Taiwanese experts were dispatched to Wuhan (apparently that evening) to carry out “pathogen detection and investigation of the cause of infection.” (Taiwan CDC, 2019).
Given the later political sparring over Taiwan’s WHO membership, it is important to bear in mind that Taiwan was not the last to know, but the first. It already had its own experts on the ground in Wuhan that day or the next. And it had the Wuhan report to China’s WHO office in hand before formal transmission to the WHO headquarters in Geneva.
When the Chinese Public Knew
What was known in mainland China? The Hong-Kong-based South China Morning Post article of 31 December includes the following information (note especially the reference to “state television”):
“State television reported that a team of experts from the National Health Commission had arrived in Wuhan to lead the investigation, while People’s Daily said the exact cause remained unclear and it would be premature to speculate.
People’s Daily also quoted several hospital sources in the city who said it was likely that the virus responsible was different from SARS, which infected more than 5,300 people and killed 349 in mainland China between late 2002 and mid-2003.” (emphasis added)
China’s business press reported that “A reporter from China Business News called the official hotline 12320 of the Wuhan Municipal Health Commission on the morning of the 31st to learn that the content of the document was true. The staff of the 12320 hotline said that the type of pneumonia of unknown cause that occurred in Wuhan this time has yet to be ascertained.” (see ISID, 2019 for links).
The South China Morning Post article also notes that the Wuhan authorities’ report of the 30 December was circulating on Chinese social media:
“News of the outbreak in Wuhan came to light after an urgent notice from the city’s health department, which told hospitals to report further cases of “pneumonia of unknown origin,” started circulating on social media on Monday night [30 December].”
Note that in the original reporting, the social media reports are not described as leaks but are social media posts passing on an “urgent notice from the city’s health department” to hospitals in Wuhan. In China, the outbreak was reported on state television, the People’s Daily, and was making the rounds on social media, based on an official notice, on 30 December.
How serious was the situation? A later report in China Youth Daily confirms that “the video of doctors crying in the office on New Year’s Eve was true” (Wang, 2020).
When the World Knew
Meanwhile, over in North America, the following commentary was posted just before midnight on 30 December on the ISID ProMed site, an organization whose job it is to monitor this type of news:
“[Having been involved in moderating the SARS-CoV (Severe acute respiratory syndrome - coronavirus) and the MERS-CoV (Middle Eastern Respiratory Syndrome - coronavirus), the type of social media activity that is now surrounding this event, is very reminiscent of the original “rumours” that accompanied the SARS-CoV outbreak. The exception is the transparency of the local government in responding to this currently undiagnosed outbreak. While this report does not contain the tweets, there have been numerous tweets about this as yet undiagnosed outbreak.” (emphasis added)
Transparency of the local government? Social media activity reporting on official notices? Experts around the world connecting this outbreak to SARS and MERS as early as 30 December 2019? This is the reality before the issue became a geopolitical hot potato.
As for official agencies, an example is provided by Canada, whose provincial health authorities were awake as well on New Year’s Eve of 2019. Here is the “Emerging Respiratory Virus Bulletin,” dated 31 December 2019, issued by British Columbia’s Centre for Disease Control. It is presented at length to provide a sense of how this news was received in Canada (note especially the sanguine commentary on the concerns about a re-emergence of SARS) and the specific references it makes to the social media postings and the twenty-seven cases mentioned in the Wuhan authorities’ report of 31 December, indicating knowledge of the information circulating in Asia that day. Note especially the phrases: “This message is to let you know we are aware,” and the reference to “routine practices” for infection control in such circumstances:
Dear Colleagues -
RE: Undiagnosed, atypical pneumonia in central China
You may have seen recent social media reports of a cluster of 27 as yet undiagnosed cases of atypical pneumonia in central China (Wuhan, in Hubei province) during December, notably involving seafood market workers (seven in critical condition). Currently, there are no reports of health care workers being affected. A viral pneumonia of unknown origin has been suggested amid much speculation, including concerns about SARS re-emergence.
This message is to let you know that we are aware and following this cluster but that SARS-related fears remain unfounded (and unlikely). Other respiratory pathogens are prevalent at this time of year, with influenza-like illness (ILI) and influenza virus activity (foremost A(H3N2)) showing a recent increase in China more generally.
We will provide updates as indicated. In the meantime, this serves as a useful reminder of routine practices that include travel history and appropriate infection control precautions for all patients presenting with severe acute respiratory illness. Clinicians should consult their Medical Health Officer, infection control practitioner and/or Medical Microbiologist with any questions and/or for further guidance.” (BC Centre for Disease Control, 2019). (Emphasis added)
As of 31 December 2019, the news of the yet-to-be-identified pandemic-to-be was all over the world. It was on Chinese state media, in the Hong Kong press, on social media in mainland China and outside of mainland China (quoted in fact in the United States) and in official communications (e.g., in Canada). It was duly noted by agencies set up to monitor infectious diseases, duly noted by national authorities responsible for infectious disease control, and already acted on by mainland China’s closest neighbours, Hong Kong and Taiwan.
Outside of China, the opinion of both health authorities and experts appears to have been quite sanguine. Notably, the authorities in Hong Kong and Taiwan moved immediately to implement countermeasures notwithstanding the unknowns, whereas there is no indication that other authorities did more than take notice. In Europe, France took measures as of 10 January and was the first to identify a case in Europe: “Strengthened surveillance of COVID-19 cases was implemented in France on 10 January 2020, with the objective of identifying imported cases early to prevent secondary transmission in the community, and the National Reference Center for Respiratory Viruses (NRC) hosted at Institut Pasteur identified the first cases in Europe” (Gámbaro et al. 2020).
When the Genome Sequence was Known
Perhaps most importantly for the development of a vaccine, the gene sequencing of the new virus was done with extraordinary rapidity. Professor Yong-Zhen Zhang of the Shanghai Public Health Clinical Center and School of Public Health, received the virus from Wuhan on 03 January at 1:30 pm and completed the sequencing in less than two days, on 05 January at 2 a.m. (Tufekci, 2020). The genome was shared with members of Zhang’s consortium, which included Australian scientist Eddie Holmes, who posted the genome on Virological.org, with Zhang’s permission on 10 January (Tufekci, 2020). The genome was also posted at about the same time on Genbank (Cohen, 2020a).
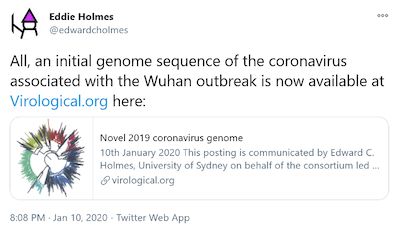
Accordingly, the genome sequence was in possession of researchers outside of China before the posting of the information globally on 10 January, the decision to post was taken outside of China as well, and international efforts to model a vaccine were underway without delay as of the time of the posting. It is important to bear in mind through all this that the very first death to be attributed to the coronavirus had not yet been reported at the time of posting (Cohen, 2020a notes that the first death was reported on 11 January).
20-20 HINDSIGHT

Obviously, before the first official reports were made by the Wuhan medical authorities, there was a period of time when there was a growing awareness that something was afoot, practitioners were connecting the dots, launching investigative processes, consulting internally, and of course developing their report. The question has been posed whether the local Wuhan health authorities and China’s national authorities, including its political leadership, should have been expected to have identified the COVID-19 outbreak earlier. This question has been answered in the affirmative – for example, a sub-headline to a Wall Street Journal article states: “China’s errors, dating back to the very first patients, were compounded by political leaders who dragged their feet to inform the public of the risks and to take decisive control measures.” (Page, Fan and Khan, 2020; emphasis added).
Based on our current understanding of the virus, here are some basic facts that need to be taken into account in formulating any opinion on how well Wuhan reacted to the challenge it faced. I emphasize that all of this information came to light over the course of 2020, but we are going to apply that information to assess the response of Wuhan authorities in late December 2019, when the very first patients were being identified and treated.
The Implications of Novelty
First, COVID-19 is novel and therefore was unknown to the first responders – in this case these were the Wuhan medical practitioners and authorities. The disease had no name, it had no unique signature in terms of symptoms, etc., and it came unannounced at a time when other viruses causing some of the same flu-like symptoms were especially active.
Here is how the Wall Street Journal described its arrival in a retrospective account published in March 2020:
“It was on 10 December that Wei Guixian, a seafood merchant in this city’s Hua’nan market, first started to feel sick. Thinking she was getting a cold, she walked to a small local clinic to get some treatment and then went back to work.
Eight days later, the 57-year-old was barely conscious in a hospital bed, one of the first suspected cases in a coronavirus epidemic that has paralyzed China and gripped the global economy” (Page et al. 2020).
Other reports elaborate on Wei’s account:
“I felt a bit tired, but not as tired as previous years,” she told Chinese news outlet The Paper, recalling her initial symptoms. “Every winter, I always suffer from the flu. So I thought it was the flu.” (reported in Brown, 2020).
On 16 December, after initial treatments failed, she checked into Wuhan Union Hospital. On 18 December she was reported as being barely conscious (Page et al., 2020). She survived to tell her story to the Chinese newspaper.
To put this in context, China has on the order of close to 90,000 flu-related excess deaths annually (Li et al., 2019), which, for a city the size of Wuhan (11 million population, equivalent roughly to the population of Los Angeles County in the United States) would be close to 700 deaths per year (compared to about 3,245 influenza and pneumonia deaths per year in Los Angeles County annually). These are deaths, not hospitalizations.
Between 16 December and 27 December (when a cluster was first identified) is a week and a half. This is dramatized by the Wall Street Journal as follows:
“For almost three weeks, doctors struggled to connect the dots between Ms. Wei and other early cases, many of them Hua’nan vendors. Patient after patient reported similar symptoms, but many, like her, visited small, poorly resourced clinics and hospitals. Some patients balked at paying for chest scans; others, including Ms. Wei, refused to be transferred to bigger facilities that were better-equipped to identify infectious diseases.” (Page et al., 2020)
Accordingly, before Wuhan identified a novel disease, we have “patient after patient” (i.e., at least 27) reporting “similar symptoms” (i.e., stubborn flu-like symptoms) to various clinics and hospitals (many poorly resourced – this is, after all, a country with a per capita GDP that is 1/6th that of the United States) in a major metropolitan area, during flu season, over a period of a week and a half (expanded ungenerously to “almost three weeks” by the Wall Street Journal reporters), with no deaths.
Wuhan’s (and by extension, China’s) diagnostic failures, by these accounts, are grave indeed. Or perhaps not. In this regard, Shao Yiming, an official at China’s Center for Disease Control and Prevention, made the following observations (reported in Cohen, 2020b):
“… when you’re first, you move from unknown to known, and then known to reaction. This takes a much longer time: You first have to rule out other known viral and bacterial pathogens from the clusters of similar pneumonia. You have to understand what’s happening and invest a lot to identify the unknown pathogen.
For all the other countries it’s totally different, since they started with a known disease and preliminary knowledge about how to control it.”
That sounds about right.
The Silence of the Spread
Because it was novel, COVID-19 initially confronted a petri dish of a population without antibody protection (this was true in every region of the world it reached) and therefore would have spread at a rate consistent with its basic reproduction number or R0 in a context of a complete absence of interventions to prevent its spread.
Nailing down the basic reproduction number or R0 is a work in progress, but it appears to be at least on the order of 2.5. This is generally in line with similar viruses such as SARS (2–5), MERS (2.7–3.9), and, indeed, the seasonal flu.
- Zhao et al. (2020) placed the R0 at 2.56 (CI of 2.49–2.63).
- Imai et al. (2020) placed it at 2.6 (CI of 1.5–3.5).
- Wu et al. (2020) placed it at 2.68 (CI of 2.47-2.86).
This means the virus spreads quite quickly through a susceptible community, as each case leads to approximately 2.5 additional cases.
The “serial interval” – the time it takes to transfer the virus to another person – is not known but based on research on similar viruses is estimated at about a week (Wu et al., assumed 8.4 based on SARS in Hong Kong and report an estimate of 7.5 days based on China CDC data). This means an infected person interacts with numerous people while only infecting a few, meaning the connections may be difficult to establish. By the same token, the gradual invasion and spread through contacts, including between asymptomatic individuals and fresh targets, is likely to be spread over an extended period of time before a significant cluster of clearly connected infections emerges to announce its presence and cause health authorities to take precautions.
A number of other factors combine to give COVID-19 a “stealth” character – i.e., to allow it to spread silently. These factors include the following:
- It takes some time to incubate before symptoms become apparent. The mean incubation period for the virus is estimated by Wu et al. (2020) to be 6 days, consistent with estimates for SARS and MERS and also data on COVID-19 from China CDC. Qin et al. (2020) place the mean at 8.29 days. As these are mean figures, accordingly, many individuals will have longer incubation periods: Qin et al. put the 90% percentile at a little over 14 days and the 99th percentile at almost 3 weeks (also, Guan et al., put an upper limit of 24 days).
- It is contagious before symptoms are expressed. An infected individual is contagious for a significant time while the virus is incubating before symptoms emerge. The share of “virus shedding”, which is the viral load emitted by an individual which serves to transmit the virus to new hosts, by a pre-symptomatic individual is estimated by one study to be 44% of the total shedding by that individual (He, Xi et al. 2020). This study found that infectiousness started about 2.5 days before symptom onset, peaked at 0.6 days before symptom onset, and declined relatively quickly within 7 days of illness onset. Early viral load peak helps explains the efficient community spread of COVID-19 compared to cases of SARS and MERS, in which community spread was brought under control quickly, and also the relatively few cases of hospital outbreaks (Cevik et al., 2020); the latter observation helps explain the early non-finding in Wuhan of transmission to health-care personnel in the early stages of the outbreak in that region.
- It generates severe symptoms that require hospitalization in only a small percentage of the infected population. The majority of symptomatic cases are relatively mild and produce symptoms associated with common colds and respiratory conditions. Only a relatively small minority of cases is severe enough to require hospitalization. In British Columbia, only 11% of documented cases as of 25 March 2020 resulted in hospitalization. Accordingly, about 90% of the actual cases are likely to fly under the medical system radar until randomized testing is initiated to determine the true extent of the spread of the virus.A statistical epidemiological modeling study that attempted to reconstruct the outbreak in Wuhan over the period from 1 January 2020 to 8 March concluded that up to 87% of cases in the city during that time may have gone undetected (Siliezar, 2020). The same would have applied in the period prior to identification of the virus in late December.
- It presents with a variety of symptoms that would not necessarily be connected by medical professionals. For example, the initial reports out of Wuhan focussed on the main symptoms of pneumonia, as did the initial medical reports elsewhere when the pandemic spread. It took some time for medical practitioners to connect the coronavirus to additional symptoms such as loss of taste, other neurological impacts, hypoxia in patients with no difficulty breathing, heart problems, rashes and “Covid toes”, and perhaps others. As of August 2020, the loss of taste and extreme fatigue are thought to be the most common expressions of the disease.
- It is hard to trace because it transmits through aerosols and the virus is viable for several hours in this form. In a laboratory study, the virus remained viable in aerosols throughout the duration of the 3-hour experiment with a half-life of approximately 1.1 to 1.2 hours as the median estimate, and with 95% credible intervals of 0.64 to 2.64 hours (van Doremalen et al., 2020). This enables it to drive super-spreading events, including the Seattle choir practice (Read, 2020), the Korean church service (Lanese, 2020), and the Bergamo football match (Robinson, 2020). Aerosol transmission compromises the ability of tracing initiatives since physical distancing is not enough to fully protect if an individual is shedding virus in a closed public space. The virus also remains viable for several hours on various types of surfaces, although that is now being downplayed as a vector of transmission.
If the full spectrum of symptoms and the characteristics of the disease had been known to Wuhan health authorities in December 2019, they might very well have identified the presence of COVID-19 earlier and attenuated the impact in China at an earlier stage. But that is, of course, not what they knew then. That is what we know now.
The Delay of Morbidity
Deaths start to occur perhaps a month after the initial infection. The mean time to death from the first expression of symptoms in critical patients is about 18 days. Accordingly, even after the hospitals start to accumulate patients, lethality is not likely to be established immediately. Further, the fact that fatalities typically involve co-morbidities in older persons creates an obvious identification problem. The fact that deaths can occur for reasons unrelated to pneumonia complicates things further in terms of establishing lethality – and in alerting medical authorities as to the severity of an outbreak.
The deadliness as measured by the case fatality rate (CFR) is high enough to eventually cause the body bags to accumulate to a level that drives political reaction but small enough to give the virus time to run rampant. The virus is currently estimated to be 10 times more deadly than influenza.
The use of “excess deaths” to measure the likely true impact of COVID-19 on any given region only started several months after the pandemic emerged (regular reporting of this started in the mainstream western media only in May 2020). Notably, He, Mai et al. (2020), a study first posted end of May 2020, provides links to contemporary news coverage in China on 31 January of suspected cases not being included in the official statistics because patients were turned away due to hospitals being full. This study also concludes, based on analysis of excess deaths (using urn counts and expanded operating times for crematoriums in Wuhan) starting on or about 25 January, that the death toll in Wuhan was as much as 36,000, or more than 10 times the official total of 2,524 for the period covered by their study.
The Virus Travelled Incognito – and Travelled Widely
China has a surveillance mechanism for reporting by local hospitals of “pneumonia of unknown etiology.” According to available information, the first identification of a situation was on 27 December when three connected cases of unknown pneumonia were reported by Dr. Zhang Jixian (Cohen, 2020b). Another published report indicates 4 cases as of 29 December (Li et al., 2020). The count grew to 27 as reported by the Wuhan City Health Commission.
As a digression, subsequent commentary on this figure suggested that it in fact conflicted with other official estimates.
“On December 31, 2019, the Wuhan City Health Commission announced that recent cases of pneumonia of unknown etiology seen in some hospitals were related to the Wet Market and 27 cases were found by the time. This official announcement conflicted with at least two official numbers and one media report which were 45, 104 and 266 cases.” (He, Mai et al. 2020).
These alternative figures, however, cover different periods and regions. The figure of 45 was for Wuhan as of 31 December (cited in Li et al., 2020, a study which looked at the first 425 cases in Wuhan that had been laboratory-confirmed as of 22 January 2020); the original Wuhan City Health Commission compilation could not have included cases that presented on the 31st. The figure of 104 covered cases in all of China that were identified in subsequent retrospective analysis with an onset date of December 31 or earlier and recorded in the infectious disease information system as of 11 February 2020 (Epidemiology Group, 2020). The 266 cases were all cases identified in China with onset dates in 2019 based on retrospective analysis that pushed the first infection back to 17 November (Ma, 2020).
Meanwhile, retrospective forensic analysis identified a patient in France with COVID-19 as of 27 December 2019 (Reuters, 2020). That patient had no connection with China; hence it was community spread, meaning an infection likely weeks earlier and the original infection in France at least weeks before that. Retrospective analysis has identified a patient in Colmar, France, with lung damage typical of COVID-19 based on scans taken on 16 November 2019 (Cjada and Fugler, 2020).
A virus that was spreading silently in France at the same time it was spreading silently in China was undoubtedly spreading silently in other jurisdictions as well.
- In Italy, a study testing for COVID-19 antibodies in blood samples of asymptomatic individuals enrolled in a prospective lung cancer screening trial found an unexpected very early circulation of the virus with 14% of those tested in September 2019 found to be positive (DiarioDelWeb, 2020).
- Another retrospective analysis by a team involved in the Measles and Rubella Network, which explored the possibility of COVID being the agent for a number of measles-like cases that tested negative for measles, identified one early positive case based on a swab sample. This involved a child in the Milan area who developed cough and rhinitis symptoms as of 21 November, was taken to the emergency department with respiratory symptoms and vomiting on 30 November, and developed a measles-like rash on 1 December, a pattern observed in younger COVID patients (Amendola, et al., 2021).
- Similarly, retrospective research on sewage water samples has identified early COVID-19 presence in several European cities prior to the identification of the disease, including in Barcelona between March and May 2019 (Chavarria-Miró et al., 2020) – which followed immediately upon the 2019 Mobile World Congress held on 25-28 February 2019 – and in Turin and Milan in mid-December 2019 (La Rosa et al., 2020).
- The US Centers for Disease Control and Prevention have identified COVID-19 in blood donations in December (McKay, 2020; Basavaraju et al. 2020); these results, which are not necessarily conclusive in and of themselves given the possibility of false positives and/or potential cross reactivity with human common coronavirus infection, lend support to the suspicion that COVID-19 was the cause of the spike in patients with coughs and acute respiratory failure at UCLA Health hospitals and clinics beginning in late December 2019 (Elmore et al. 2020).
Accordingly, even before the identification of the breakout in Wuhan, there is a growing body of evidence supporting the conclusion that the virus had already spread around the globe, establishing the basis for an outbreak that would draw attention to itself somewhere in the world sooner or later. The first identification happened to be Wuhan, where the first super spreader event occurred (not surprisingly in a meat market given the multiple major outbreaks in meatpacking plants), but that is actual history; alternative histories were eminently possible.
WE HAVE THE CRISIS WE CHOSE

Taken together, the characteristics of COVID-19 suggest that this virus is unusually well-positioned to start a significant pandemic: it gets around quickly enough, gets transmitted before it causes symptoms, and mostly does not lead to hospitalization, where it would attract attention. An Imperial College London study estimated (retrospectively I hasten to add given how this type of information has been presented in the press) that a total of 1,723 cases in Wuhan had developed symptoms by 12 January, with an unknown additional number of infectious asymptomatic cases. The first death attributed to COVID-19 in China was around that time, on 9 January (reported on 11 January; Cohen, 2020a). Accordingly, by the time that the first attributed fatality was registered, retrospective estimates suggest that there were already several thousand infected individuals in Wuhan. The same is likely true of France and other countries to which the virus had already spread un-noticed.
This pattern suggests that, in the first outbreak of this disease, the virus would have established itself in the attacked community before it came to the attention of medical authorities. Secondly, the severity of the illness would not have become apparent until a substantial number of cases had already started to fill the hospitals (Wang, 2020 reports that the hospitals in Wuhan were already filled by 11 January) and the death toll had risen to a level that prompted authorities to take emergency action (the first cluster of deaths in Wuhan, which provoked the shutdown of Wuhan on 23 January, occurred between the 17th and 20th of January). This was close to a month after the cluster of infections was identified as a novel disease. This means that the unlucky first location was bound to have a large outbreak. And that was Wuhan.
What is particularly notable regarding timing is that the coronavirus was gene sequenced and the information posted globally by 11 January, just days after the first death. Moreover, when the genome was posted, the global pharmaceutical community was immediately in action identifying possible vaccines. The race to find a vaccine was on even as the very first known fatality was recorded. From this perspective, the response to the outbreak was almost unbelievably good.
On the unfortunate side, the virus made its first known major outbreak in Wuhan, a commercial and transportation hub of 11 million people. An average of about 3,300 passengers left Wuhan per day in the normal course during that period (Imai et al., 2020; Report 1). Throughout the period of silent spread – which various estimates place as far back as October 2019 – the opportunity for the virus to move within China and internationally was wide open – and the virus took advantage.
The decision-making challenge for authorities that COVID-19 poses is when to take emergency action? Wuhan acted when the hospitals were full and a cluster of deaths emerged. Notably, in the SARS outbreak in Toronto, the Ontario health authorities declared an emergency only when the Toronto hospitals were filled. The Ontario account is worth reviewing at length in light of the commentaries on the speed of Wuhan’s reaction and the reporting by China’s national authorities (Low, 2004):
“On 23 March 2003, officials recognized that the number of available negative pressure rooms in Toronto was being exhausted. In a 4-hour period on the afternoon of 23 March, staff at West Park Hospital, a chronic care facility in the city, recommissioned 25 beds in an unused building formerly used to house patients with tuberculosis. Despite the efforts of West Park physicians and nurses, and assistance from staff at the Scarborough Grace and Mount Sinai Hospitals, qualified staff could be found to care for only 14 patients.
Faced with increasing transmission, the Ontario government designated SARS as a reportable, communicable, and virulent disease under the Health Protection and Promotion Act on 25 March 2003. This move gave public health officials the authority to track infected people and issue orders preventing them from engaging in activities that might transmit the new disease. Provincial public health activated its emergency operations center.
By the evening of 26 March 2003, the West Park unit and all available negative pressure rooms in Toronto hospitals were full; however, 10 ill Scarborough Hospital staff needing admissions were waiting in the emergency department, and others who were ill were waiting at home to be seen. Overnight, with the declaration of a provincial emergency, the Ontario government required all hospitals to create units to care for SARS patients.
By 25 March 2003, Health Canada was reporting 19 cases of SARS in Canada—18 in Ontario and the single case in Vancouver. But 48 patients with a presumptive diagnosis of SARS had, in fact, been admitted to hospital by the end of that day. Many more individuals were starting to feel symptoms, and would subsequently be identified as SARS patients. Epidemic curves later showed that this period was the peak of the outbreak. On 19 March, nine Canadians developed “probable” SARS, the highest single-day total. Taking “suspect” and “probable” cases together, the peak was 26 March, and the 3 days 25 March to 27 are the highest 3-day period in the outbreak.
The Ontario government declared SARS a provincial emergency on 26 March 2003. Under the Emergency Management Act, the government has the power to direct and control local governments and facilities to ensure that necessary services are provided.”
To recap: in Toronto, with SARS, the hospital system was stressed, with inadequate beds in negative pressure rooms and too few health care staff for the SARS patients, as of 23 March 2003. The Ontario government designated SARS as a reportable, communicable, and virulent disease under the Health Protection and Promotion Act, a full two days later on 25 March 2003. At the national level, there was significant under-reporting as of this date, with only 18 cases reported for Ontario, although 48 patients had been admitted with presumptive cases of SARS. And it was not until another day, when the Toronto hospital system was overflowing, emergency had a line-up, and ill people were waiting at home that the Ontario Government declared a provincial emergency.
With COVID-19, jurisdictions ranging from Sweden to the United Kingdom to the United States declined to take early decisive emergency actions, such as were adopted (for example) by New Zealand, as case counts rose. As an epidemiologist observed in remarking on the management of the pandemic as cases started to rise again in August 2020: “Lack of deaths = lack of action.” (Hodcroft, 2020).
If another jurisdiction had been the first to experience a breakout, what can one conclude about its responses? Consider this report (retrospective, I hasten to add) from a doctor in Alsace, France:
"Nous avions tous été frappés (intrigués, ndlr) cet automne par des épisodes grippaux un peu bizarres, qui ont duré plus longtemps que d'habitude, avec plus de douleurs, plus de température, plus de fatigue … On avait un à deux patients par semaine, au tout début. Ensuite sont arrivés les fêtes de Noël et les marchés de Noël et il y a eu un peu plus de contagions. Et tout a démarré vraiment chez nous, à Colmar, le 6 mars.”
Translation . . .
“We had all been struck (intrigued, editor’s note) this fall by somewhat bizarre flu episodes, which lasted longer than usual, with more pain, more temperature, more fatigue … We had one or two patients per week, at the very beginning. Then came the Christmas celebrations and the Christmas markets and there was a little more contagion. And everything really started with us, in Colmar, on 6 March” (Cjada and Fugler, 2020).
As the sanguine reactions of experts and government authorities show, most jurisdictions would not likely have acted much earlier or more decisively than China – and certainly not those jurisdictions that have declined to act decisively even when confronted with death tolls rising to the tens and now the hundreds of thousands. What is important to recognize is that the first jurisdiction could have been almost anywhere in the world.
There are several key conclusions to be drawn from this review.
- First, there was no “information asymmetry” across countries concerning the outbreak in Wuhan at the time that policy decisions had to be taken. There was, for all intents and purposes, almost instantaneous transmission of the key information around the world – even before the formal notices through official WHO channels – and a global sharing of the genome sequence in record time through professional channels on the authority of the professionals themselves.
- Second, the policy-relevant information on hand as of 31 December 2019 concerning that outbreak was sufficient to frame the necessary preventative responses and fully anticipate what today is regarded as best practice.
- Third, regardless of the timing and rigour of the responses to the Wuhan outbreak in Wuhan and China more generally, global transmission was a sealed deal because of the stealth nature of COVID-19.
The pandemic was probably not preventable. Moreover, the scale of the pandemic is a function of policy choices made independently by governments and health experts around the world based on the same and sufficient information. We all have the COVID-19 crisis that we “chose” through our governance mechanisms.
References
Amendola, Antonella, Silvia Bianchi, Maria Gori, Daniela Colzani, Marta Canuti, Elisa Borghi, Mario C. Raviglione, Gian Vincenzo Zuccotti, and Elisabetta Tanzi. 2021. “Evidence of SARS-CoV-2 RNA in an oropharyngeal swab specimen, Milan, Italy, early December 2019,” Emerging Infectious Diseases 27(2), February. https://doi.org/10.3201/eid2702.204632
BC Centre for Disease Control. 2019. “Emerging Respiratory Virus Bulletin – December 31, 2019,” http://www.bccdc.ca/health-professionals/data-reports/communicable-diseases/emerging-respiratory-virus-updates
Basavaraju, Sridhar V., Monica E. Patton, Kacie Grim2, Mohammed Ata Ur Rasheed, Sandra Lester, Lisa Mills, Megan Stumpf, Brandi Freeman, Azaibi Tamin, Jennifer Harcourt, Jarad Schiffer, Vera Semenova, Han Li, Bailey Alston, Muyiwa Ategbole, Shanna Bolcen, Darbi Boulay Peter Browning, Li Cronin, Ebenezer David, Rita Desai, Monica Epperson, Yamini Gorantla, Tao Jia, Panagiotis Maniatis, Kimberly Moss, Kristina Ortiz, So Hee Park, Palak Patel, Yunlong Qin, Evelene Steward-Clark, Heather Tatum, Andrew Vogan, Briana Zellner, Jan Drobeniuc, Matthew RP Sapiano, Fiona Havers, Carrie Reed, Susan Gerber, Natalie J. Thornburg, and Susan L. Stramer. 2020. “Serologic testing of U.S. blood donations to identify SARS-CoV-2-reactive antibodies: December 2019-January 2020,” Clinical Infectious Diseases, ciaa1785, 30 November. https://doi.org/10.1093/cid/ciaa1785
Brown, Natalie. 2020. “‘Patient zero’ at Wuhan market identified,” The Chronicle, 27 March.
Campbell, Don. 2020. “How does COVID-19 spread? U of T infectious disease expert breaks down the latest research,” U of T News, University of Toronto, 30 July. https://www.utoronto.ca/news/how-does-covid-19-spread-u-t-infectious-disease-expert-breaks-down-latest-research
Cevik, Muge, Julia L. Marcus, Caroline Buckee, and Tara C Smith. 2020. “SARS-CoV-2 transmission dynamics should inform policy,”, 14 September. Available at SSRN: https://ssrn.com/abstract=3692807
Chavarria-Miró, Gemma, Eduard Anfruns-Estrada, Susana Guix, Miquel Paraira, Belén Galofré, Gloria Sánchez, Rosa M. Pintó, and Albert Bosch. 2020. “Sentinel surveillance of SARS-CoV-2 in wastewater anticipates the occurrence of COVID-19 cases,” medRxiv preprint doi: https://doi.org/10.1101/2020.06.13.20129627
Chun, Han Wong. 2020. “Health Secretary Alex Azar Renews Swipes at China Over Coronavirus in Taiwan Visit,” Wall Street Journal, 11 August.
Cohen, Jon. 2020a. “Chinese researchers reveal draft genome of virus implicated in Wuhan pneumonia outbreak,” Science, 11 January. https://www.sciencemag.org/news/2020/01/chinese-researchers-reveal-draft-genome-virus-implicated-wuhan-pneumonia-outbreak
Cohen, Jon. 2020b. “ ‘The house was on fire.’ Top Chinese virologist on how China and U.S. have met the pandemic,” Science, 22 May.
Cjada, Maud and Corinne Fugler. 2020. “Coronavirus: un premier cas dès le mois de novembre en Alsace,” France Bleu, 7 May. https://www.francebleu.fr/infos/sante-sciences/coronavirus-un-premier-cas-des-le-mois-de-novembre-en-alsace-1588830642
DiarioDelWeb. 2020. “The coronavirus has been circulating in Italy since September 2019,” DiarioDelWeb, 16 November.
Elmore, Joann G. Pin-Chieh Wang, Kathleen F. Kerr, David L. Schriger, Douglas E. Morrison, Ron Brookmeyer, Michael A. Pfeffer, Thomas H. Payne, Judith S. Currier. 2020. “Excess Patient Visits for Cough and Pulmonary Disease at a Large US Health System in the Months Prior to the COVID-19 Pandemic: Time-Series Analysis,” Journal of Medical Internet Research 22 (9). e21562 DOI: 10.2196/21562
Epidemiology Group of Emergency Response Mechanism of Novel Coronavirus Pneumonia, Chinese Center for Disease Control and Prevention. 2020. “Analysis of Epidemiological Characteristics of Novel Coronavirus Pneumonia[J],” Chinese Journal of Epidemiology 41(02): 145-151. DOI: 10.3760/cma.j.issn.0254-6450.2020.02.003
Hodcroft, Emma. 2020. Twitter post, 19 August. https://twitter.com/firefoxx66/status/1296080778934329347
Imai, Natsuko, Anne Cori, Ilaria Dorigatti, Marc Baguelin, Christl A. Donnelly, Steven Riley, and Neil M. Ferguson. 2020. “Transmissibility of 2019-nCoV,” Report 3, WHO Collaborating Centre for Infectious Disease Modelling, MRC Centre for Global Infectious Disease Analysis, Abdul Latif Jameel Institute for Disease and Emergency Analytics (J-IDEA), and Imperial College London.
ISID. 2020. “Undiagnosed Pneumonia - China (Hubei): Request for Information,” International Society for Infectious Diseases, ProMED-mail post, http://www.promedmail.org, 30 December 2019.
Gámbaro, Fabiana, Sylvie Behillil, Artem Baidaliuk, Flora Donati, Mélanie Albert, Andreea Alexandru, Maud Vanpeene, Méline Bizard, Angela Brisebarre, Marion Barbet, Fawzi Derrar, Sylvie van der Werf, Vincent Enouf and Etienne Simon-Loriere. 2020. “Introductions and early spread of SARS-CoV-2 in France,” bioRxiv preprint doi: https://doi.org/10.1101/2020.04.24.059576.
Guan, Wei-jie, Zheng-yi Ni, Yu Hu, Wen-hua Liang, Chun-quan, Jian-xing He, Lei Liu, Hong Shan, Chun-liang Lei, David S.C. Hui, Bin Du, Lan-juan, Guang Zeng, Kwok-Yung Yuen, Ru-chong Chen, Chun-li Tang, Tao Wang, Ping-yan Chen, Jie Xiang, Shi-yue Li, Jin-lin Wang, Zi-jing Liang, Yi-xiang Peng, Li Wei, Yong Liu, Ya-hua Hu, Peng Peng, Jian-ming Wang, Ji-yang Liu, Zhong Chen, Gang Li, Zhi-jian Zheng, Shao-qin Qiu, Jie Luo, Chang-jiang Ye, Shao-yong Zhu, and Nan-shan Zhong. 2020. “Clinical characteristics of 2019 novel coronavirus infection in China,” dRxiv preprint, 9 February. doi: https://doi.org/10.1101/2020.02.06.20020974,.
He, Xi, Eric HY Lau, Peng Wu, Xilong Deng, Jian Wang, Xinxin Hao, Yiu Chung Lau, Jessica Y Wong, Yujuan Guan, Xinghua Tan, Xiaoneng Mo, Yanqing Chen, Baolin Liao, Weilie Chen, Fengyu Hu, Qing Zhang, Mingqiu Zhong, Yanrong Wu, Lingzhai Zhao, Fuchun Zhang, Benjamin J Cowling, Fang Li, and Gabriel M Leung. 2020. “Temporal dynamics in viral shedding and transmissibility of COVID-19,” doi: https://doi.org/10.1101/2020.03.15.20036707
He, Mai, Li Li, Louis P. Dehner, and Lucia F. Dunn. 2020. “Cremation based estimates suggest significant under- and delayed reporting of COVID-19 2 epidemic data in Wuhan and China,” medRxiv preprint, 16 June. doi: https://doi.org/10.1101/2020.05.28.20116012.
Keitner, Chimène. 2020. “The Foreign Sovereign Immunities Act, Coronavirus, and Addressing China’s Culpability,” Testimony to the United States Senate Committee on the Judiciary, 23 June 2020.
La Rosa, Giuseppina, Pamela Mancini, Giusy Bonanno Ferraro, Carolina Veneri, Marcello Iaconelli, Lucia Bonadonna, Luca Lucentini, and Elisabetta Suffredini. 2020. “SARS-CoV-2 has been circulating in northern Italy since December 2019: evidence from environmental monitoring,” medRxiv preprint doi: https://doi.org/10.1101/2020.06.25.20140061.
Lanese, Nicoletta. 2020. “'Superspreader' in South Korea infects nearly 40 people with coronavirus,” Live Science, 23 February.
Lester, Simon. 2020. “China Should Embrace a Coronavirus Investigation. Here’s Why,” National Interest (Online), 28 April.
Li, Li, Yunning Liu, Peng Wu, Zhibin Peng, Xiling Wang, Tao Chen, Jessica YT Wong, Juan Yang, Helen S. Bond, Lijun Wang, Yiu Chung Lau, Jiandong Zheng, Shuo Feng, Ying Qin, Vicky J. Fang, Hui Jiang, Eric HY Lau, Shiwei Liu, Jinlei Qi, Juanjuan Zhang, Jing Yang, Yangni He, Maigeng Zhou, Benjamin J. Cowling, Luzhao Feng, and Hongjie Yu. 2019. “Influenza-associated excess respiratory mortality in China, 2010-15: a population-based study,” Lancet Public Health 4(9): e473-e481. doi:10.1016/S2468-2667(19)30163-X
Li, Qun, Xuhua Guan, Peng Wu, Xiaoye Wang, Lei Zhou, Yeqing Tong, Ruiqi Ren, Kathy S.M. Leung, Eric H.Y. Lau, Jessica Y. Wong, Xuesen Xing, Nijuan Xiang, Yang Wu, Chao Li, Qi Chen, Dan Li, Tian Liu, Jing Zhao, Man Liu, Wenxiao Tu, Chuding Chen, Lianmei Jin, Rui Yang, Qi Wang, Suhua Zhou, Rui Wang, Hui Liu, Yinbo Luo, Yuan Liu, Ge Shao, Huan Li, Zhongfa Tao, Yang Yang, Zhiqiang Deng, Boxi Liu, Zhitao Ma, Yanping Zhang, Guoqing Shi, Tommy T.Y. Lam, Joseph T. Wu, George F. Gao, Benjamin J. Cowling, Bo Yang, Gabriel M. Leung, and Zijian Feng. 2020. “Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia,” New England Journal of Medicine 382(13), March: 1199–1207.
Low, Donald E. 2004. “SARS: Lessons From Toronto,” in Stacey Knobler, Adel Mahmoud, Stanley Lemon, Alison Mack, Laura Sivitz, and Katherine Oberholtzer (eds), Learning from SARS: Preparing for the Next Disease Outbreak – Workshop Summary. National Academies Press: 63-71.
Ma, Josephine. 2020. “Coronavirus: China’s first confirmed Covid-19 case traced back to November 17,” South China Morning Post, 13 March. https://www.scmp.com/news/china/society/article/3074991/coronavirus-chinas-first-confirmed-covid-19-case-traced-back
McKay, Betsy. 2020. “Covid-19 Likely in U.S. in Mid-December 2019, CDC Scientists Report,” Wall Street Journal, 30 November. https://www.wsj.com/articles/covid-19-likely-in-u-s-in-mid-december-2019-cdc-scientists-report-11606782449?mod=e2tw
OCAC. 2020. “How Taiwan has been able to keep COVID-19 at bay,” Overseas Community Affairs Council, 17 March. https://www.ocac.gov.tw/OCAC/Eng/Pages/Detail.aspx?nodeid=329&pid=15730946
Page, Jeremy, Wenxin Fan and Natasha Khan. 2020. “How It All Started: China’s Early Coronavirus Missteps,” Wall Street Journal, 6 March.
Qin, Jing, Chong You, Qiushi Lin, Taojun Hu, Shicheng Yu, and Xiao-Hua Zhou. 2020. “Estimation of incubation period distribution of COVID-19 using disease onset forward time: A novel cross-sectional and forward follow-up study,” Science Advances 6: 1-7, 14 August.
Read, Richard. 2020. “A choir decided to go ahead with rehearsal. Now dozens of members have COVID-19 and two are dead,” Los Angeles Times, 29 March.
Reuters. 2020. “French hospital discovers Covid-19 case from December,” Reuters, 4 May.
Robinson, Joshua. 2020. “The Soccer Match that Kicked Off Italy’s Coronavirus Disaster,” Wall Street Journal, 1 April.
Siliezar, Juan. 2020. “Study suggests undetected cases help speed COVID-19 spread,” Harvard Gazette, 16 July. https://news.harvard.edu/gazette/story/2020/07/study-finds-early-wuhan-covid-cases-largely-undetected/
Taiwan CDC. 2019. “In response to the outbreak of pneumonia in Wuhan, Mainland China, the Department of Disease Control continued to implement border quarantine and implement boarding quarantine for Wuhan inbound flights,” Press Release, Taiwan Center for Disease Control, 31 December. https://www.cdc.gov.tw/Bulletin/Detail/zicpvVlBKj-UVeZ5yWBrLQ?typeid=9
Tufekci, Zeynep. 2020. “The Pandemic Heroes Who Gave us the Gift of Time and Gift of Information,” Blogpost, Substack.com, 30 November. https://zeynep.substack.com/p/the-pandemic-heroes-who-gave-us-the
van Doremalen, Neeltje, Trenton Bushmaker, Dylan H. Morris, Myndi G. Holbrook, Amandine Gamble, Brandi N. Williamson, Azaibi Tamin, Jennifer L. Harcourt, Natalie J. Thornburg, Susan I. Gerber, M.D. James O. Lloyd-Smith, and Emmie de Wit. 2020. “Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1,” Correspondence, New England Journal of Medicine, 17 March.
Wang, Jiaxing. 2020. “Before Zhong Nanshan spoke, the doctor in Wuhan issued an outbreak alert to nearby schools,” China Youth Daily, 28 January.
Wu, Joseph T., Kathy Leung, and Gabriel M. Leung. 2020. “Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study,” The Lancet 395: 29 February 29.
Zhao, Shi, Salihu S. Musa, Qianying Lin, Jinjun Ran, Guangpu Yang, Weiming Wang, Yijun Lou, Lin Yang, Daozhou Gao, Daihai He, and Maggie H. Wang. 2020. “Estimating the Unreported Number of Novel Coronavirus (2019-nCoV) Cases in China in the First Half of January 2020: A Data-Driven Modelling Analysis of the Early Outbreak,” Journal of Clinical Medicine 9: 388. doi:10.3390/jcm9020388
Zuo, Mandy, Lilian Cheng, Alice Yan, and Cannix Yau. 2019. “Hong Kong takes emergency measures as mystery ‘pneumonia’ infects dozens in China’s Wuhan city.” South China Morning Post, 31 December.